The idea is to introduce the body’s immune system to the virus and prime it to counter the disease if it subsequently encounters the same virus. But these vaccines, known as inactivated, or live-attenuated vaccines, depending on the approach used, can take years to develop and perfect.
Appearing at the fag end of 2019, SARS-CoV-2, or the novel coronavirus, was a pathogen that the human immune system had never encountered before. As Covid-19 wreaked havoc on health systems and brought the world to a standstill, scientists and experts raced to find an urgent solution. The time was ripe for the mRNA vaccine to prove its mettle.
In Search Of Swift Solutions
The ‘m’ in mRNA stands for ‘messenger’ and sums up the principle on which these vaccines work. The development of these vaccines owes to recent advancements in the field of molecular biology. Instead of introducing the whole virus into the human body, these vaccines work by inserting individual viral components that can stimulate the immune system. These components are mainly “parts of the viral genetic code, usually encoding proteins found on the virus surface”, says the Nobel Foundation. These surface proteins are what the virus normally uses to invade and latch on to the cells of a human host.
The bit of genetic code that is delivered by the viral component serves to spur the production of proteins that stimulate the formation of virus-blocking antibodies. And it is the antibodies that drive the body’s fight against a virus.
A well-known example of a vaccine based on this approach is the one against the hepatitis B virus. But producing vaccines based on whole viruses, or their proteins – vector-based vaccines, the type developed against Ebola also belong to this category – requires extensive infrastructure and involves a resource-intensive process. Which means that the scope for rapid development, as was required under the novel coronavirus attack, is limited. mRNA vaccines are designed to overcome these hurdles. But for a long time, there weren’t many takers for it.
A Shot Of Hope
The DNA in human cells contains the information for making proteins and is a key building block of life. But as Shurjo Sen, programme director with the US National Human Genome Research Institute, says it is the RNA that is “the actual functional form of nucleic acids… (for) constructing cells or responding to immune challenges”. Importantly, mRNAs are essential as “the form in which a gene gets read by the cell”. While scientists thought of utilising mRNA for creating vaccines there were issues to address. Simply put, mRNA vaccines were regarded as being unstable and difficult to deliver and also gave rise to inflammatory reactions.
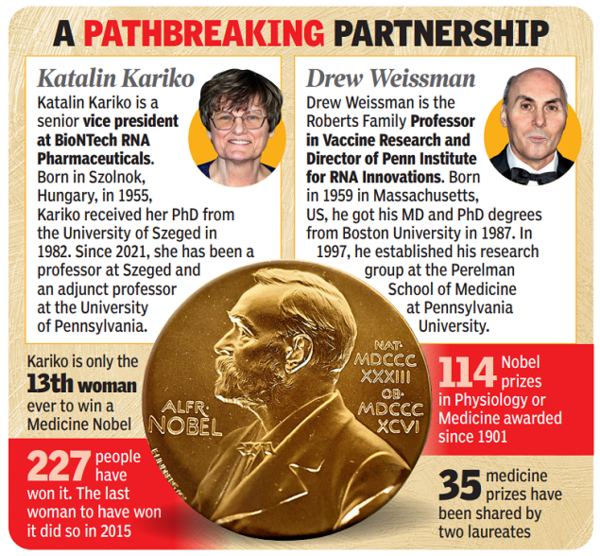
But Katalin Kariko, an assistant professor at the University of Pennsylvania in the US in the early 90s, stayed steadfast to the idea of using mRNA for therapy even though it was a challenge to convince funders to back her research. She soon found an ally in immunologist Drew Weissman. He was working on dendritic cells that are key to immune surveillance and triggering vaccine-induced immune responses.

The duo found that in vitro, or lab-developed mRNA, are recognised by dendritic cells as a foreign substance, triggering inflammation. The clue, they thought, likely lay at the level of bases contained in nucleic acids, that is DNA and RNA. “They wondered if the absence of altered bases in the in vitro transcribed RNA could explain the unwanted inflammatory reaction,” says the Nobel Foundation. They then set about coming up with different variants of mRNA after chemically altering their bases.
Their experiment showed that when the bases were modified, the inflammatory response almost disappeared. They published their results in 2005.
Kariko and Weissman subsequently found that mRNA generated with base modifications increased protein production while also inhibiting inflammatory responses, the two factors that had hindered the development of mRNA vaccines.
Thereafter, mRNA research picked up pace and vaccines for Zika virus and MERS-CoV were explored using this method. MERS-CoV-2 is similar to SARSCoV-2 and, so, when the pandemic broke, two mRNA vaccines, the first ever, were developed at lightning speed by Pfizer-BioNTech and Moderna. These vaccines were found to induce a strong immune response. Moreover, mRNA vaccines have shorter manufacturing times and are considered safe because they do not contain a live virus.

