Bhubaneswar: A light brown-coloured building, landscaped gardens, aesthetically designed interiors, a small water body within the premises, and wards named after flowers in Odia — with this backdrop, the Bagchi Karunashraya Palliative Care Centre has begun partial operations. Odisha’s first such facility, with a capacity of 110 beds, provides free healthcare to poor, terminally ill cancer patients to ease their suffering during the final stages.
The first in-patient ward of the Rs 80-crore centre was opened last month. “The entire facility with 16 wards, eight doctors and 100 nurses, nurse aides and counsellors will become fully operational by July,” Gurmeet Singh Randhawa, managing trustee of the Bangalore Hospice Trust, which runs Bagchi Karunashraya, told ThePrint.
Randhawa said the idea behind opening the centre was to provide quality palliative care completely free of cost to patients, mostly from low-income backgrounds, approaching the end of life. The only requirement is a certification from a doctor that the patient is terminally ill and needs end-of-life care.

The centre, built by the Bangalore Hospice Trust with a donation of Rs 130 crore from entrepreneurs Sushmita and Subroto Bagchi, has come up on a 22-acre plot of land given by the Odisha government in Bhubaneswar’s Pokhariput.
Mindtree co-founder Subroto Bagchi is also the chief advisor on institutional capacity building to the Odisha government. Bangalore Hospice Trust is a public charitable trust jointly formed in 1994 by the Indian Cancer Society’s Karnataka Chapter and Rotary Bangalore Indiranagar, to provide palliative care to terminally ill patients. It runs mainly through individual donations as well as CSR funding from corporates.
The Bagchi Karunashraya centre offers outpatient department (OPD) as well as inpatient services. Patients can consult doctors, get free medication and avail daycare services in the OPD, while in the inpatient ward, terminal cancer patients can get admission with services like nursing, doctor consultation, physiotherapy and counselling, besides medication and food.
Currently, a team of six doctors, three counsellors and 40 nursing staff, apart from the administrative staff, are working at the facility. “Our general ratio even in Bangalore is 1:1 for nurses to patients,” Randhawa said.
The nursing staff have been provided with housing facilities within the premises. “They have dormitories and are also provided with free food. Currently, doctor and staff quarters are being constructed,” said Saroj Kumar Ghadei, public relations manager at Bagchi Karunashraya.

A team of dedicated counsellors — an integral part of palliative care — cater to the psychological, social and spiritual needs of not just the patients and their caregivers, but also doctors, nurses and staff members. Keshav Sharma, who heads the counselling services at the centre, told ThePrint that while the physical pain is taken care of by doctors and nurses via medication, counsellors have a difficult job.
“Counselling a patient who knows he is going to die is extremely difficult. There is this fear of death, which we term as death anxiety. Then people have a fear of unfulfilled businesses… If they die, who will look after their children… There is anger… why did God do this, what have I done wrong to deserve this… all this is taken care of by my team here,” Sharma said.
Besides the patient, the counsellors also provide their services to the primary caregivers, comprising the patient’s family. Sharma added that a caregiver’s distress, which is actually as stressful as a patient’s distress, also needs to be addressed.
After a patient dies, Karunashraya makes arrangements for the last rites and other rituals.
Dr Praveena Karnam, associate medical director and palliative care specialist at the centre, said that once a patient is admitted, the doctors first try to stabilise his symptoms. “Then the patient is sent back to home care, where he is tended to by the home care team. As and when the patient’s symptoms worsen, he or she is admitted again,” she explained.
The Bagchi Karunashraya has also been running a homecare service for the past three years. There are two teams of doctors and nurses who visit the patients’ homes. These patients are referred by various hospitals.
“It was part of the Bagchi Karunashraya Palliative Care Centre, but since we did not have the facility earlier, it was running on its own. And now, of course, it’s running from the centre premises. We are known in the hospitals in Bhubaneswar through our homecare,” Randhawa said.
Then there are also those patients at the end of their lives who are admitted and taken care of. “We ensure that he/she gets a good death,” Dr Karnam said.
She explained that by “good death”, they do not mean that they are not trying to make anything negative or positive. “Death is negative and remains negative, but if death comes in a bad way, then that is what is left in the survivor’s mind. Anytime they think about the patient, they only remember how bad the death was. So, the ‘good’ death is not only for the patient, but for the survivors also. They are left with the thought that the patient did not at least have a painful end. This helps the survivor in coping with the loss of his loved one,” she added.
The hospice has been landscaped keeping in mind the patient’s general frame of mind. “You will see a lot of greenery and a water body inside the premises. The idea is that when a patient gets depressed and stressed out, he or she can come to these diversional therapy spaces. Doctors at the hospice say water brings positive vibes,” Ghadei said.

Even the wards at the centre have been given the names of flowers in Odia — champa, malli, kia, kadam among others.
The palliative care facility has been set up next to the Bagchi Sri Shankara Cancer Hospital, which, with 750 beds, is one of the biggest cancer hospitals in the country.
Now, the Karunashraya Institute of Palliative Care and Research is also coming up at the premises. This will impart training to doctors, nurses and nurse aides about palliative care services.
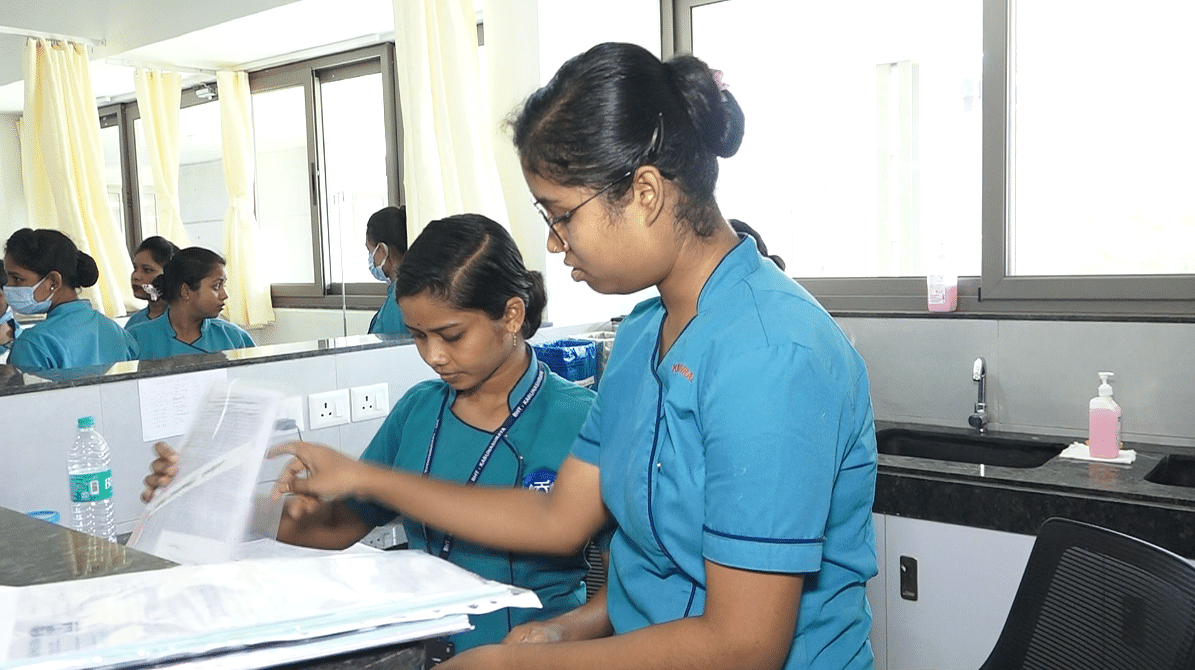
The training for nursing assistants is free. “Tribal girls are provided free training here. 65 of the total nursing staff at the facility currently, who have been trained here, are from backward tribal areas,” said Ghadei.
Also Read: Central regulator to now give NOC for export of new, unapproved medicines after safety concerns
The inception of the centre
Managing trustee Randhawa recalled that the process of building the centre first started in 2021, when the Bagchis came looking to donate money for cancer treatment and palliative care. “Mr Bagchi had helped us with our strategy plan some years ago. He knew our organisation well. He asked us if we would be interested in setting up a palliative care centre in Bhubaneswar… So we said yes and then the Odisha government was very welcoming and gave us land… So it all fell into place,” he elaborated.

A tripartite agreement between the Bangalore Hospice Trust, Odisha government and the Bagchis, who were to fund the facility, was signed. “Once we took over the land, we started construction in 2022, and in April 2024, we took in our first patient,” he added. Plans to open a second ward by the end of June are in the works.
The trust is also interacting with hospitals, oncologists and onco-surgeons and spreading the word about the facility, so that they refer their patients there. “These things are happening simultaneously. By mid-July, we should be fully functional,” said Randhawa.
The majority of the staff members at the centre are from Odisha.
Palliative care in India
Palliative care is not a new concept, but in India, there is limited awareness and proliferation. The first such service in India came about in 1985 in Mumbai.
There are anywhere between 1,200 and 1,250 facilities in India providing end-of-life care currently, a majority of them in Kerala.
Dr M.R. Rajagopal, founder of Kerala-based Pallium India, which provides palliative care and effective pain relief for terminal patients, said that even now, 39 years since the inception of the first such service in India, end-of-life care reaches less than 1 percent of the population.
The National Health Policy of 2017 deems palliative care a part of primary care. It is included in undergraduate medical and nursing education now. In 2021, it was added to BSc nursing courses.
“Even basic pain management reaches less than 4 percent of the population of India. The progress has been so slow, but I do believe that we are on a steep path of the growth curve, mainly because of these policy and education changes,” Dr Rajagopal, chairman emeritus, Pallium India told ThePrint.
Dr Rajagopal, considered by many to be the father of palliative care in India, added that it goes hand in hand with investigations and treatment aimed at cure in relevant cases, and for terminal patients, it continues as relief from suffering until the end of life.
“It extends to the bereavement phase for the caregivers. Hospice is an important part of the larger whole… What is happening in Odisha is a great, great, divine moment but along with that, the message should be that it must be an integral part of all healthcare,” he said, adding that there is a need to create more awareness around palliative care.
“There is a feeling that we have concentrated on creating policies and educating the professionals but did not realise that we need to reach out to people who need it. They have to be aware.”
(Edited by Mannat Chugh)
Also Read: Decision not to hold NEET super speciality exam this year sparks concerns among PG doctors

