Bengaluru: The World Health Organisation (WHO) has once again declared Mpox (formerly known as monkeypox) as a public health emergency in Africa. The disease first made its appearance in 1970, and was mostly contained to the continent. However, the last outbreak that originated in Nigeria in the second half of 2022 had spread through the world.
The current outbreak, which has been raging since early this year, is a clade (or variant) localised to the African continent. Multiple African countries have detected a large number of cases with the central part of the continent being the hotspot.
As of today, over 17,000 Mpox Clade 1 cases have been reported in Africa, with just over 500 fatalities. The Democratic Republic of Congo (DRC) has seen the most cases, exceeding 8,000 this year, with over 350 deaths in May.
“We declare today this public health emergency of continental security to mobilise our institutions, our collective will, and our resources to act swiftly and decisively,” Africa Centres for Disease Control and Prevention Director General Jean Kaseya said in a press briefing Tuesday.
Two clades of Mpox have been reported. Clade 2 has typically been observed in central Africa, but it’s the more severe Clade 1 that seems to be spreading this time. Apart from the DRC, which has reported spread of the Clade 1b strain of Mpox, East African countries of Kenya, Uganda, Rwanda, and Burundi have reported cases for the first time. This has led to concerns of a stronger and more transmissible variant emerging here.
What is Mpox, how contagious is it, and how risky is to the rest of the world? ThePrint explains.
Also Read: India may soon get 1st dengue vaccine, but wait for jab effective against all 4 strains could be longer
What is Mpox and where does it occur?
Mpox is an infectious disease first detected in monkeys, leading to its earlier name monkeypox. However, the name was considered a misnomer as monkeys are not the primary hosts of the virus. Additionally, the name also led to racist connotations and stigma against the disease in Africa, which led to its renaming to Mpox in November 2022.
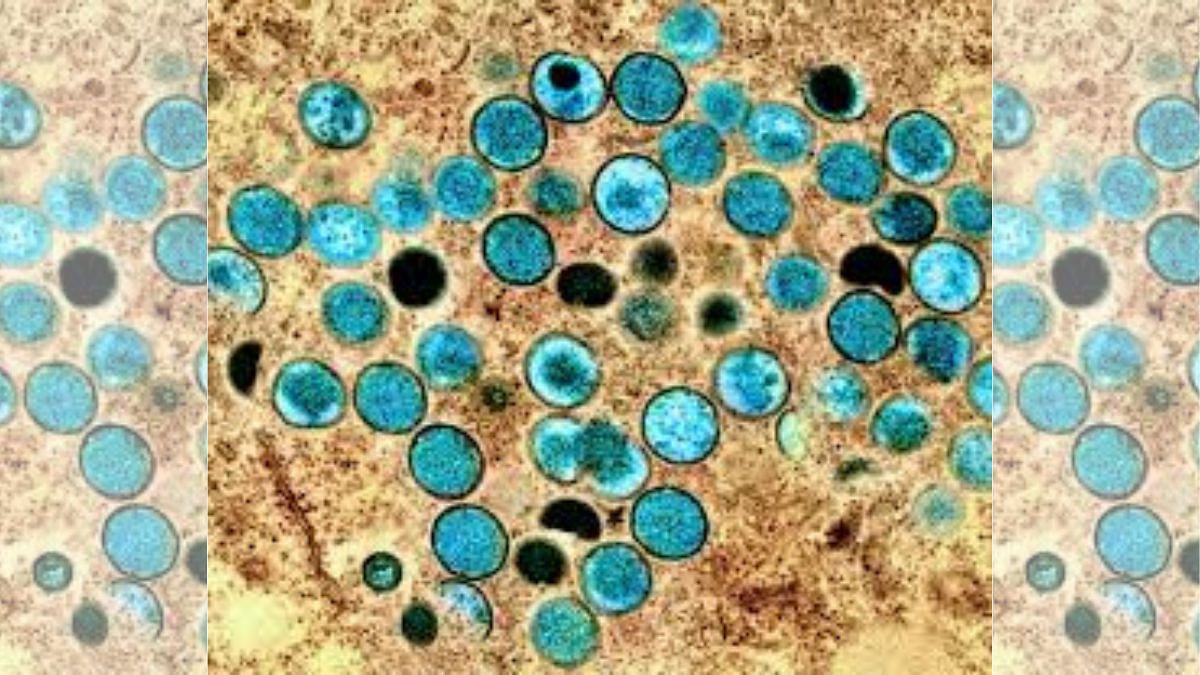
Mpox is spread by the monkeypox virus, which is related to the smallpox family. It is a zoonotic disease, having emerged in other animals and jumped to humans. Associated diseases in the family are smallpox, cowpox, horsepox, and camelpox. It has two variants, Clade 1 is more severe, while Clade 2 is now becoming more widespread around the globe.
It is contagious among humans and can transmit through direct contact with infected skin or bodily fluids. It can spread from touch, sexual contact, handling of infected meat, or by bites or scratches from an infected animal.
MPox is endemic to central and western Africa, and is thought to occur in multiple species of mammals on the continent. The first case among humans was diagnosed in 1970 in the DRC, after which the disease has increased in both frequency and severity.
A global outbreak first occurred as recorded by community transmission outside of Africa in 2022-2023, likely due to the lowering of related smallpox vaccination rates, as the disease has been eradicated in humans.
The disease has been detected in almost all other countries, and other species today, including dogs. The first case outside of Africa was recorded in the United States in 2003.
What are its symptoms?
Mpox symptoms start to show about 4-10 days after infection, as a rash or lesions on palms and feet, face, mouth, and genitals. These can fill with fluid and pus, and disappear after a few days, similar to chickenpox bumps.
It can also be asymptomatic in many, and can last up to 21 days inside the body, causing illness and infection. It is often accompanied by fever, body and muscle ache, and excessive fatigue.
In more severe cases, it can lead to encephalitis (swelling of the brain), pneumonia (filling of lungs with fluid), sepsis (infection in the bloodstream), blindness, and complications in future pregnancies. About 1 percent of cases result in death, and these are primarily among individuals who are immunocompromised such as those with cancer or HIV.
Most infected people recover in 2-4 weeks.
The incubation period for the virus inside the body can be anywhere from 1 to 20 days, and it is treated promptly by vaccine administration.
How can Mpox be prevented and treated?
The disease is both prevented and treated with the MVA-BN vaccine, which was originally developed for smallpox, administered before or after infection.
Those living in Mpox-endemic countries, as well as in regions where there is an outbreak, are advised to avoid contact with stray and farm animals, non-human primates, and wild animals — both dead and alive. People at risk are also advised to wear masks, gloves, and goggles.
Which countries are at risk today for Mpox?
Mpox has been found in most countries including the Americas, Australia, all of Europe, Asia and Southeast Asia, and the Indian subcontinent after the November 2022 outbreak, originating out of Nigeria. Three new cases have reportedly been confirmed in the US.
The current emergency has only been declared inside of Africa, and there is a spread of Clades 1, 1b, and 2 in 12 countries there. Clade 1 is the most widely prevalent in the current outbreak in Africa.
Outside of Africa, Clade 2 is still expected to be present in low amounts and transmission, but nothing has been recorded yet in this outbreak. The risk of infection today exists for those travelling to and from central and eastern African nations, as well as those coming in contact directly or indirectly with animals there.
(Edited by Gitanjali Das)
Also Read: India seeing worst Chandipura virus outbreak in over 2 decades. Here’s what you need to know