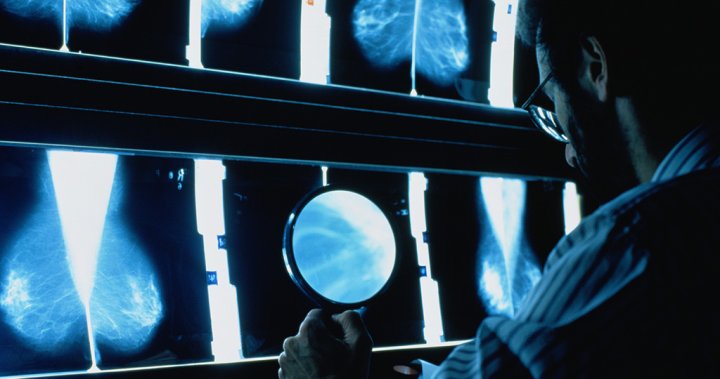
A new AI tool for mammograms is expected to help doctors and health-care providers move faster and more efficiently catch breast cancers in patients.
Health Canada approved the technology, ProFound Risk, earlier this summer amid a health-care crunch that has seen hospitals, specialists and providers across the country pushed to the breaking point and straining to meet demand over recent years.
The device uses artificial intelligence (AI) to provide patients with personalized risk estimations, even when a current mammogram comes back clear. It was founded by American technology company iCAD, which specializes in breast cancer detection and therapy solutions.
iCAD’s founder and CEO, Dana Brown, says the device can dramatically change a patient’s care pathway once breast cancer risk is detected.
“The peace of mind that this technology can give both the patient and the provider to be on the right path for the next two years and be very vigilant about it, I think is just amazing,” Brown told Global News.
Brown explains that the device not only detects the risk of cancer, but also where it may appear specifically within the body. Both details are important for providers to best keep tabs on a patient and provide guidance on lifestyle risk mitigators such as diet and exercise.
Brown says it’s also “empowering” for individuals to be able to take control of their own health.
“Cancer is often something you feel you have no control over,” she said.
Breast cancer accounts for approximately 25 per cent of new cancer cases and 13 per cent of cancer deaths in Canadian women, according to the Government of Canada website.
One in eight women are expected to develop breast cancer during their lifetime, and one in 33 will die of it.
“We’re thrilled that the Canadian regulatory bodies see the urgent need and worked with us to get this technology approved for use because I think it can make a huge difference in saving more lives, and it’s something that’s really needed for Canadian women,” Brown said.
The new mammogram has a higher area under the curve (AUC) than other risk assessment devices, which is a measurement used to show accuracy of these technologies.
1.0 is considered a perfect score. While other devices land around the 0.60 mark, ProFound Risk has a score of 0.80.
Canadians are expected to have access to the ProFound Risk mammogram in the next one to two years.
The machine, which is available for both 2D and 3D mammography, has also been cleared for use in the European Union. The device is offered in the United States, but currently only for investigational purposes.
How the AI-mammogram has changed lives
Dr. Mark Traill is one of the radiologists part of the investigational study. He’s been using the device for five years while overseeing the artificial intelligence development in the University of Michigan Health-West’s radiology department.
Traill has been working in the industry for 35 years, but he says it wasn’t until he witnessed iCAD’s device in action that he saw the true value of AI in radiology.
“In this time, what I assumed was going to be the outcome has (come true): that artificial intelligence algorithms are extremely capable at picking out cancer on a mammogram,” Traill told Global News.
“The amount of stress that I have during the day, looking at literally thousands of pictures is much less now because I know I’ve got an algorithm looking at the images with me that actually is going to pick up 90-plus per cent of the cancers I’m going to see that day,” he said.
Traill says his net performance in finding cancer has increased since using the AI-powered mammogram.
“For me, being able to see a score change in the risk category is telling me, ‘Hey, something’s happening in this breast that could indicate cancer is on the horizon,’” he said.
According to Traill, cancer is missed on a mammogram 10 to 30 per cent of the time when read only by humans.

One experience has especially stood out to Traill, he says.
He says a woman once came to him complaining of fullness, but mentioned that her toddler had been banging his head repeatedly on her chest. Traill performed a precautionary mammogram which came back clear, but her risk score was incredibly high.
Traill told her to come back for another mammogram in three months. When she returned, not only was the risk score higher, but there were very small findings of cancer.
“If I had not had the risk score available, I would have written this off as trauma with some swelling and bruising,” Traill said.
“I didn’t do it in this case so we were able to get ahead… and get her into treatment before it got too far along.”
The device isn’t the first risk model out there, but it’s the only one not to base results on genetic histories. Traill says the latter models don’t address the vast majority of women that are at risk.
Only about five to 10 per cent of breast cancers are hereditary, according to the U.S. Centers for Disease Control and Prevention (CDC).
Traill says it’s also beneficial that the device doesn’t rely on human input — where patients have to recall their family history — because the information isn’t always accurate. Instead, the AI in ProFound Risk uses an algorithm directly part of the mammogram to analyze risk.
Previous models also only provide a lifetime risk assessment of breast cancer, but knowing one’s short-term risk allows them to better plan and make changes to their lifestyles accordingly.
Traill says it’s been a challenge to get more radiologists on board with using AI in their practice.
“There’s a real bias in radiologists at times against it. You need to develop a trust with the algorithm as in any type of relationship, and that takes time,” Traill says.
“But from what I’ve experienced over the years, it’s indispensable. I would never practice without it,” he says.
Traill also says it’s important for both radiologists and patients to realize that AI is not replacing doctors, but rather acts as a “complementary function.”
“Humans just can’t do it (alone), is the bottom line in the studies,” he says.

Advancements in AI for breast cancer solutions
AI has been making big leaps in breast cancer detection and treatment in recent years.
A recent early-stage study in The Lancet Oncology found that AI is a safe and efficient tool for breast cancer detection and boosting the accuracy of diagnoses.
The AI in the study was able to cut doctor mammogram screen-reading workload almost in half, by 44.3 per cent.
A study published in January 2020 by the journal Nature also found that AI can more accurately predict breast cancer than humans.
The AI reduced false positives by 5.7 per cent in the U.S. and 1.2 per cent in the U.K. datasets. It also reduced false negatives by 9.4 per cent in the U.S. and 2.7 per cent in the U.K., meaning it picked up on cancers that humans had missed.
Alexander Wong, professor and Canada Research Chair in Artificial Intelligence and Medical Imaging at the University of Waterloo, is part of a lab out of Waterloo, Ont., working to help patients get proper treatment with new AI-driven technology.
“It’s actually quite exciting,” Wong said about ProFound Risk.
“AI does help a lot, but that said, there’s still a lot of information that’s not being leveraged, so that’s where the clinician really comes in to actually use these technologies as a second opinion or as additional information to help them treat patients better,” he told Global News last week.
Wong also says there are intangible pieces of information useful for assessing risk that only doctors might experience when treating a patient.
“So that’s where the combination of the clinician… plus the AI can really yield a benefit,” he said.
Traill says he would recommend that patients avoid mammography centres that don’t use some sort of AI.
“I think it’s super important that women know that this is an option for them.”
Traill says he’s very excited about the future.
“I don’t think there’s any way that this is not the future of diagnostic radiology.”